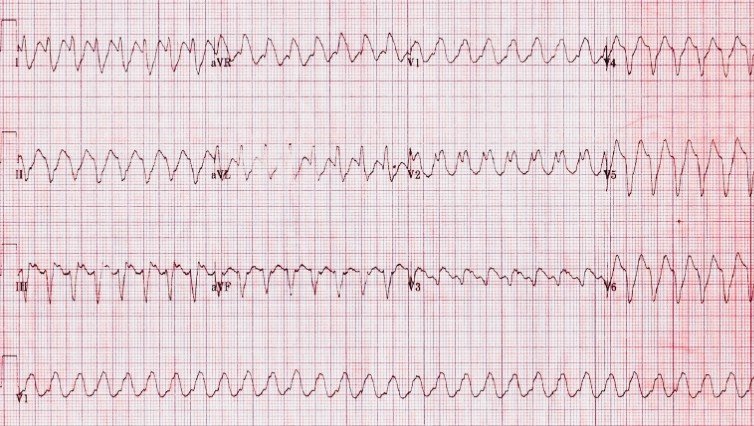
A 3-year-old boy with repaired tetralogy of Fallot (RVOT patch + transannular patch) is admitted to the cardiac ICU with worsening fatigue and presyncope. He is postoperative day 5 following pulmonary valve replacement. He suddenly develops a regular wide-complex tachycardia at 220/min, with MAP decreasing to 45 mmHg despite fluid bolus. Near-infrared spectroscopy demonstrates declining cerebral and renal saturations, lactate increases to 5.2 mmol/L, and central venous pressure acutely rises. Temporary pacing wires are in situ. A 12-lead ECG is shown.
Quiz Question
What is the most likely ECG diagnosis, and what is the immediate priority in management?
Diagnosis
Sustained Monomorphic Ventricular Tachycardia
ECG features supporting VT:
⦁ Broad QRS tachycardia (>160 ms)
⦁ Regular rhythm with uniform QRS morphology
⦁ Extreme axis deviation
⦁ Absence of consistent P-QRS relationship (AV dissociation)
⦁ Post-surgical substrate with RV scar–related reentry
Physiologic & Clinical Risks
⦁ Abrupt reduction in RV and LV filling → acute low cardiac output syndrome
⦁ RV ischemia and worsening ventriculo-arterial uncoupling
⦁ Progression to ventricular fibrillation or electrical storm
⦁ High mortality risk in repaired TOF due to:
⦁ RV dilation
⦁ Surgical scar-related reentry circuits
⦁ Postoperative inflammation and electrolyte shifts
Management Strategy (Expert-Level)
Immediate priorities: treat hemodynamics and rhythm simultaneously
Hemodynamically unstable VT:
⦁ ⚡ Immediate synchronized cardioversion
⦁ 1–2 J/kg (do not delay for drugs)
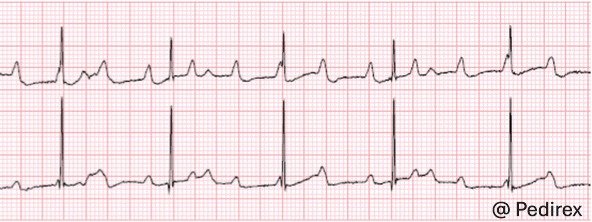
Post-conversion ICU strategy:
⦁ Initiate amiodarone infusion (or lidocaine if ischemic VT suspected)
⦁ Aggressive correction of:
⦁ K⁺ >4.0 mmol/L
⦁ Mg²⁺ >2.0 mg/dL
⦁ Optimize RV loading:
⦁ Avoid excessive preload
⦁ Reduce RV afterload (optimize ventilation, avoid hypercarbia)
⦁ Utilize overdrive pacing if recurrent VT and wires present
⦁ Early EP involvement for substrate-based VT mapping/ablation planning
Escalation:
⦁ Refractory VT → deep sedation, intubation
⦁ Consider VA-ECMO for electrical storm with cardiogenic shock
Pearls
⦁ Post-TOF VT is almost always scar-mediated reentry
⦁ Adenosine has no therapeutic role and may cause dangerous delay
⦁ Rising CVP + falling NIRS during VT suggests RV failure physiology