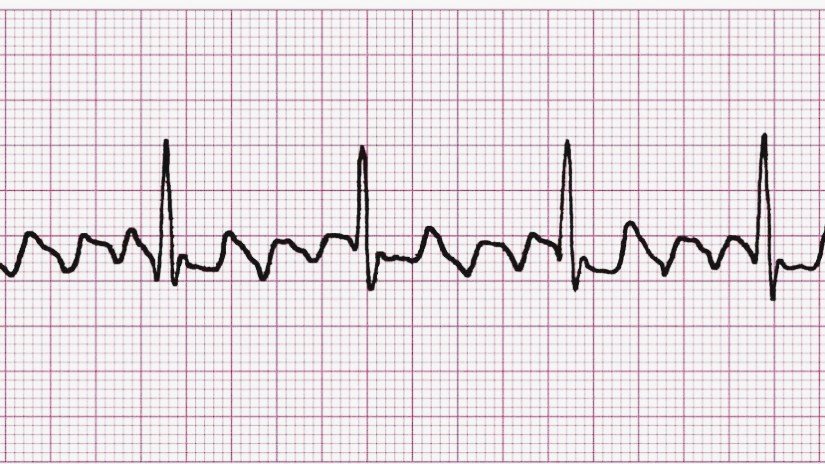
A 6-year-old child on postoperative day 2 after atrial septal defect repair develops sudden tachycardia with a heart rate of 160–170/min. Blood pressure is stable but trending downward. The monitor shows a regular narrow-complex tachycardia. The child is irritable with mild hepatomegaly and rising lactate. Adenosine transiently slows the ventricular rate, but the tachycardia immediately recurs. A 12-lead ECG rhythm strip is shown above.
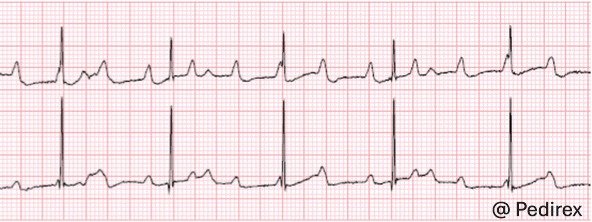
Diagnosis: Atrial Flutter with 2:1 AV conduction
ECG hallmarks:
⦁ Regular narrow QRS complexes
⦁ Ventricular rate ~150–170/min
⦁ Classic “sawtooth” flutter (F) waves, best appreciated between QRS complexes
⦁ Atrial rate ~300/min
⚠️ Clinical Risks (Especially in Pediatric Cardiac ICU)
⦁ Reduced ventricular filling → low cardiac output
⦁ Rapid decompensation in postoperative or ventricular dysfunction patients
⦁ Thromboembolism risk if prolonged (>48 hours)
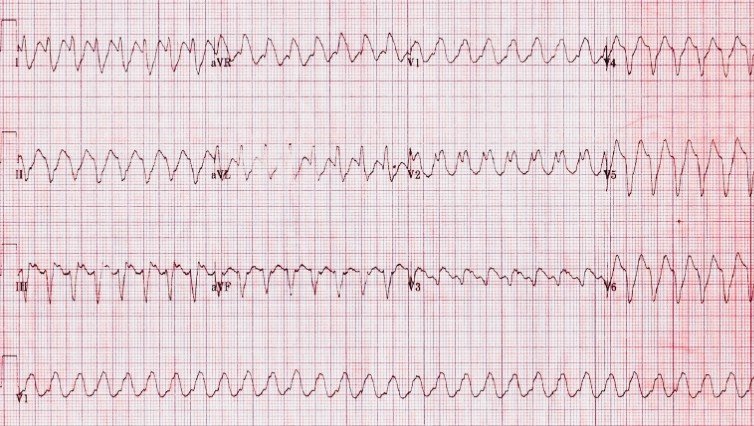
⦁ Can progress to 1:1 conduction → life-threatening tachycardia
⦁ Often resistant to adenosine (diagnostic, not therapeutic)
Management Principles
Immediate priorities depend on hemodynamic status:
⦁ If unstable (hypotension, shock, LCOS):
⦁ ⚡ Synchronized DC cardioversion (0.5–1 J/kg, escalate as needed)
⦁ If stable:
⦁ Rate or rhythm control
⦁ Amiodarone or procainamide (institutional preference)
⦁ Overdrive atrial pacing (very effective in post–cardiac surgery patients)
⦁ Consider anticoagulation if duration >48 hours or unclear onset
⦁ Optimize electrolytes (K⁺, Mg²⁺), oxygenation, and preload
Postoperative prevention:
⦁ Treat atrial stretch, inflammation, electrolyte imbalance
⦁ Vigilant monitoring in high-risk congenital heart disease patients
Teaching Pearl
Adenosine does NOT terminate atrial flutter but it can unmask flutter waves by increasing AV block. If the rhythm comes back immediately after adenosine, think atrial flutter or atrial tachycardia, not AVNRT.